Download the full letter here: https://www.gov.ie/en/collection/ba4aa0-letters-from-the-cmo-to-the-minister-for-health/#2021
(Please excuse any formatting issues, the below text is a copy/paste from the above letter.)
Dear Minister,
I write further to today’s meeting of the COVID-19 National Public Health Emergency Team (NPHET). The NPHET reviewed the latest epidemiological data, and the following key points were noted:
Epidemiological update
- A total of 12,206 cases have been reported in the 7 days to 18th October 2021 (cases to midnight 17th October), which is a 22% increase from last week when 9,998 cases were notified in the 7 days to 11th October, and a 36% increase from the last NPHET meeting on 16th September when 8,966 cases were reported in the 7 days to 15th September 2021.
- As of 18th October, the 14-day incidence rate per 100,000 population has increased to 466; this compares with 395 a week ago and compares with 402 reported at the last NPHET meeting on 16th September.
- Nationally, the 7-day incidence/100,000 population as a proportion of 14-day incidence/100,000 population is 55%, demonstrating that there have been more cases in the last 7 days compared with the preceding 7 days.
- The 5-day rolling average of daily cases is 1,736 as of today, which is a 10% increase from 1,578 a week ago (11th October) and a 43% increase from that reported at the last NPHET meeting on 16th September (1,212).
- Of the 22,204 cases notified in the past 14 days to midnight 17th October 2021, 64% have occurred in people under 45 years of age; and 13% were aged 65 years and older. With relatively even levels of vaccination across all age groups, the median age of cases (36 years) is approaching the median age of the population (38 years) indicating that risk of infection is evenly distributed across the population.
- Of the 9,533 cases reported in the latest available epi-week (Week 40 ending 9th October 2021), 5.0% (472) were healthcare workers and 2.0% (188) were determined to be travel-related. Additional data on healthcare worker status and transmission source for COVID-19 cases is currently sourced using data collected from the COVID Care Tracker (CCT).
- From the 7th – 13th October, there have been approximately 142,356 laboratory tests reported in community, private and acute laboratories. The 7-day test positivity rate in the community
was 12%. - From the 8th – 14th October, there were c. 114,049 community referrals. Overall, total referrals have increased by 6% in comparison to the same time-period last week. From the 7th – 13th October, the group with the largest number of referrals was the 4-12-year-old age group. The detected rate for the 4-12-year-old age group is 9.4%.
- According to the Contact Management Programme (CMP), from 4th – 10th October 2021, the total number of close contacts was 23,473, an increase of 16% on 20,240 the previous week. The average number of cases managed per day increased from 1,279 to 1,530, an increase of 20%.
- Of the 17,210 close contacts with self-reported vaccination status recorded, 55.7% (n=9,583) were fully vaccinated and considered to be significantly protected, an increase from 51.9% the previous week.
- The mean number of close contacts per case (including cases with zero close contacts) for the week ending 10th October was 2.4, the same as the previous week (week ending 3rd October).
- There were 482 confirmed COVID-19 cases in hospital this morning, compared with 400 last week
on 11th October, and with 290 on the morning of the last NPHET meeting on 16th September. There
have been 42 newly confirmed cases in hospital in the 24 hours preceding this morning.
- There are currently 73 confirmed cases in critical care as of this morning, compared with 75 last week on 11th October, and with 67 on the morning of the last NPHET meeting on 16th September.
There were 5 new admissions in the 24 hours preceding this morning.
- Of the 402 COVID-19 patients admitted to ICU between 1st April and 9th October 2021, 123 had
received either one or two doses of vaccine, and 82 had an epidemiological date 14 days or more
after receiving all recommended doses of vaccine.
- As of 10th October 2021, there have been a total of 5,306 COVID-19 related deaths notified in
Ireland. This is an increase of 26 notified deaths since the previous weekly update on 6th October. To date, 35 deaths have been notified which occurred in October 2021, 136 in September, 73 in August, 20 in July, and 17 in June.
- There were 54 hospital acquired COVID-19 cases in the week ending 3rd October, compared with 21 in the previous week. The substantial increase in hospital acquired cases of COVID-19 in the week ending October 3rd related to a large degree to two large acute hospital outbreaks that together account for over half of the reported cases.
- In total, 77 cases of Beta (B.1.351) and 32 cases of Gamma (P.1) have been confirmed through whole genome sequencing in Ireland as of 15th October 2021.
- Other cases of variants of interest investigation that have been confirmed in Ireland as of 15th October: 245 B.1.1.318, 7 Epsilon (B.1.429), 4 Lambda (C.37), 4 Mu (B.1.621), 2 B.1.1.7 with E484K mutation and 2 A.27.
- TaqPath S-gene PCR target results by specimen week show that the prevalence of S-gene positivity (proxy for Delta) was 98.4% in week 36.
Outbreaks and associated cases for week 40 are based on those reported up to midnight on 9th October 2021. Week 40 refers to 3rd – 9th October 2021. Additional data for week 41 (10th-16th October 2021) are included for healthcare settings and vulnerable populations.
Healthcare setting outbreaks:
- There were 13 new nursing home outbreaks with 123 confirmed linked cases and 1 community
hospital/long-stay unit outbreaks with 3 confirmed linked cases reported in week 40. There were
also 13 nursing home outbreaks reported in week 41.
- There were 10 new acute hospital outbreaks with 37 confirmed linked cases reported in week 40.
There were 13 new outbreaks reported in week 41 with 52 linked cases.
- There were 5 new outbreaks reported in residential institution settings (2 in centres for disabilities, 1 in a homeless facility, 1 in a prison and 1 in a women/ children’s refuge facility) with 16 confirmed linked cases in week 40. There were 10 new outbreaks reported in residential
institution settings in week 41; they were all in disability settings with 43 linked cases.
- There were 7 new outbreaks in ‘other healthcare services’ with 15 linked cases in week 40.
Outbreaks associated with school children and childcare facilities:
- There were 2 outbreaks newly reported in childcare facilities in week 40.
- There were 3 outbreaks reported in schools in week 40 (2 in primary schools and 1 in a special
education school) with 15 confirmed linked cases.
Workplace outbreaks:
• There were 19 workplace outbreaks reported in week 40 across a variety of settings. Of these, 4
were in the construction sector, 5 were related to food/meat production and processing settings, 8 in other types of workplaces (including office, commercial, manufacturing, health and dental and defence/justice/emergency services) and 2 were in “not-specified” workplace types.
Outbreaks associated with hospitality settings:
• There were 3 outbreaks associated with a public house, 1 with a guesthouse/B&B and 1 associated
with restaurant/café settings reported in week 40.
Other locations:
• The remaining 111 outbreaks in week 40 were across a number of other locations:
o 3 related to social gatherings;
o 1 associated with religious/other ceremony; o 1 related to retail outlets;
o 11 extended family outbreaks;
o 83 private house outbreaks;
o 9 in community outbreaks;
o 1 associated with travel;
Additional details are available in relation to outbreaks in vulnerable groups and key populations:
- There were 19 new outbreaks reported involving members of the Irish Traveller community in
week 40 with 87 linked cases. There were 10 outbreaks in this group in week 41
- There were 2 outbreaks associated with the Roma community with 15 confirmed linked cases
reported in week 40.
- There was 1 outbreak associated with the homeless with 2 confirmed linked cases in week 40.
- There was 1 outbreak in clients of mental health services with 2 linked cases in week 40
- There was 1 outbreak in third level students with 9 confirmed linked cases in week 40.
- There was 1 outbreak in a direct provision centre in week 41.
Disease incidence across the country is high and increasing. The national 7-day average of daily cases |
has increased from 1,258 two weeks ago, to 1,744 as of today, while the 14-day incidence per 100,000 population has increased from 378 to 466 over the same time period. Incidence is increasing across all age groups including those aged 65 years and older. Demand for testing remains high, and is |
increasing, and test positivity is also increasing across all age groups, with the exception of those aged 0-4 years. The total number of confirmed cases of COVID-19 in hospital has increased over the last four weeks and was 482 as of this morning, while the number of daily admissions and newly confirmed cases in hospital has increased to an average of 56 per day. Cases in hospital are growing at +2.3% (range +1.9% to +2.8%) per day. In addition, the number of COVID-19 cases in ICU and the number requiring mechanical ventilation have increased. There is currently an average of 5 COVID-19 admissions to ICU per day. Deaths related to COVID-19 are relatively constant at approximately 5 per day. Further, in recent weeks there has been a significant number of outbreaks reported in settings with vulnerable populations, such as nursing homes, as well as a recent increase in hospital acquired infections and this continues to be closely monitored. With relatively even levels of vaccination across all age groups, the median age of cases (36 years) has |
increased over recent weeks and is approaching the median age of the population (38 years) indicating that risk of infection is evenly distributed across the population. |
The July 2021 wave of Delta infections caused a subsequent increase in numbers of COVID-19 cases in hospital. However, in September, numbers in hospital increased before an increase in cases. This is because the age mix of cases changed in September, with a greater proportion of cases in older people more likely to require hospital care with longer lengths of stay. The full effect of the recent increase in cases on numbers in hospital will be seen over the next few weeks. The number of hospital admissions per 1000 cases ranged from 30 to 50 prior to the implementation of the national vaccination programme, to a low of about 20 hospitalisations per 1000 cases in July 2021 when older adults and those at higher risk of hospitalisation were vaccinated and most cases were aged under 35 years. However, this ratio has increased again to approximately 35 admissions per 1000 cases now that young adults are vaccinated, and cases are more evenly distributed across age groups. In summary, the epidemiological situation in Ireland indicates a worsening disease profile with the future trajectory very uncertain. |
Modeling update |
You will recall that the Irish Epidemiological Modelling Advisory Group (IEMAG) presented a detailed set of scenario models at the end of August (outlined in my letter of 27 August 2021). These models examined how the disease might spread in different age groups.
Given that over 90% of adults are fully vaccinated, a key determinant of the spread of infection is the extent to which unvaccinated children transmit the virus. The models examine two fundamental scenarios, one where it is assumed that children and adults are equally likely to become infected and to transmit the virus, and one where it is assumed that children under 12 years of age are 50% as likely to transmit the virus as adults (low child transmission).
Within these scenarios, the models looked at a progressive increase in effective social contact in September and October 2021:
- a conservative scenario, where effective social contact at the end of October 2021 is similar to to that seen in December 2020, but with the population maintaining basic non- pharmaceutical measures (such as self-isolating when symptomatic, good respiratory and hand hygiene, and masks in crowded settings) sufficient to interrupt about 30% of potential transmissions; and
- a pessimistic scenario where effective social contact at the end of October 2021 reverts to pre-pandemic levels with few or no effective mitigation measures.
It should be noted that ‘effective social contact’ in these models is an estimate not only of the level of close social contact, but also the risk of transmission associated with those contacts, including the effectiveness of non-pharmaceutical interventions, and the changing risk of social contact in the winter compared to the summer.
The actual case counts, numbers in hospital, and numbers requiring critical care have, since the end of August 2021, followed relatively closely the ‘low child transmission’ scenario. This accords with the international evidence that, at a population level, children transmit SARS-CoV-2 less effectively than adults. However, since early October 2020, case counts are following the more pessimistic scenario in terms of effective social contact, albeit about a week later than in the models, as has the number of people in hospital.
If we continue to track this pessimistic scenario, daily case counts are likely to increase to a peak of between 2,500 and 3,000 cases per day in the course of November, with approximately 170,000
additional cases between now and the end of the year. If this occurs, we could expect a peak of 800- 1,000 people in hospital in late November, of whom 150-200 would require critical care, with approximately 2,000 new admissions to hospital and over 300 admissions to ICU between now and the end of the year.
Latest ECDC Rapid Risk Assessment, 16th update 30th September
The latest ECDC rapid risk assessment has stated that it expects countries with high vaccination coverage could experience a manageable disease burden at current contact rates, but this disease burden would increase if contact rates increase further. Moreover, even in countries with high vaccination coverage, a high disease burden is possible due to potential waning of vaccine effectiveness or low levels of natural immunity. The ECDC recommend the following continuing measures:
- increase vaccine coverage – with particular focus on hard-to-reach population groups;
- continuation of NPIs such as the use of face masks, improved ventilation in closed spaces
and physical distancing measures;
- risk communication activities with a focus on role of COVID-19 and influenza vaccines, the
role of basic NPIs, and targeted messaging to vulnerable groups regardless of vaccination
status of the importance of adhering to NPIs;
- continuing high levels of prevention and preparedness are required in the educational
system;
- continuing importance of COVID-19 surveillance systems and genomic sequencing of
samples.
For countries with high vaccine coverage, it has assessed the current risk as follows: Risk assessment for the general population:
- Fully vaccinated people are at low risk: the probability of infection is moderate with a low impact of infection.
- Unvaccinated people are at moderate risk: the probability of infection is high with a moderate impact of infection.
Risk assessment for vulnerable populations:
- Fully vaccinated people are at moderate risk: the probability of infection is moderate with
a high impact of infection.
- Unvaccinated people are at high to very high risk: the probability of infection is high with
a very high impact of infection.
Managing the Next Phase(s) of the COVID-19 Response
As outlined in my letter of 25th August, the NPHET concluded that it may be appropriate for the public health management of COVID-19 in Ireland to transition, in broad terms, from a focus on regulation and population wide restrictions to a focus on public health advice, personal judgement and personal protective behaviours. The NPHET advised that a number of criteria should be met to progress with this transition (involving a balanced assessment on a collective basis), namely:
- At least two weeks having passed from the attainment of at least 90% vaccination uptake (i.e. completion of vaccination) in the population aged 16 years and older; and
- A point in time assessment that incidence, reproduction number, growth rate, impact and progression of infection to severe disease give confidence that we can suppress the infection sufficiently to minimise the harm of disease; and
- Hospital and critical care occupancy for COVID-19 are reducing and/or reduced to low levels to protect the health service and ensure the continued provision of non-COVID health and social care services, including in the community; and
- Public health capacities, which will need to be subject to review and an agreed plan, including in relation to testing, contact tracing, outbreak management, surveillance and sequencing for COVID-19, will be sufficiently robust to enable the rapid identification, investigation and management of local or regional outbreaks, outbreaks among vulnerable groups, and the emergence of new variants; and
- The absence of a new variant of concern with significantly increased potential for one or more of the following: greater transmissibility, increased virulence, or vaccine escape.
The NPHET has also stressed that the progressive de-escalation of public health restrictions to date has been cautious, gradual, and phased, with – crucially – sufficient time between phases to assess the impact. This approach has been critical to ensuring the protection of those most vulnerable, and the protection of health and social care, education, and childcare services. The NPHET reiterated its position that, based on past experiences, we cannot predict with certainty the future trajectory of the disease and emphasised the importance of continued monitoring in this regard. It was further cautioned that we cannot fully rule out the reintroduction of measures in the future and that we must continue to ensure our response is agile and flexible, with an ability to pivot rapidly and respond to any emerging threat. Indeed, it has always been the NPHET’s position that the public health management of the COVID-19 pandemic must evolve in light of changing circumstances, risks, and emerging evidence, and this will remain the case over the coming months.
The NPHET met earlier today to consider whether we could safely proceed with our planned transition in approach to the public health management of COVID-19, having due regard to the transition criteria as agreed on 25th August.
The NPHET concluded that the epidemiological situation has deteriorated and is now uncertain and precarious. The NPHET further concluded that the transition criteria as set out above that would facilitate the removal of the majority of the public health measures still in place have not been met, with a deteriorating disease profile, hospital and critical care occupancy increasing, and continuing sustained pressure on the provision of non-COVID health and social care services. It is therefore not recommended to proceed with the easing of public health restrictions on 22nd October as previously planned.
The NPHET today considered recommending a full pause on the easing of remaining economic restrictions, with a further review in 3-4 weeks’ time (a ‘pause’). However, the NPHET considered that there is unlikely to be a sufficient improvement in the disease profile over the short term and, therefore, did not believe it tenable that any pause now would result in a further easing of measures in November. The NPHET has therefore recommended that on balance:
- the remaining aspects of the hospitality, entertainment and night-time economy sector can reopen only with the full range of protective measures in place and the wide and robust implementation of the COVID-19 pass. In this regard, guidance should be developed or updated as appropriate by the relevant sectors.
- the range of public health protective measures currently in place across sectors should remain, including the appropriate use of masks, physical distancing, ventilation, and mitigation measures; the NPHET does not foresee these being removed until at least February 2022.
- there is a focus on increasing vaccination uptake in hard to reach and vulnerable populations, including a potential booster programme, to mitigate further risks to the healthcare system, which may be impacted by influenza and other respiratory viruses across the winter period;
- sector specific guidance and protocols with regard to hospitality, cultural and sporting events be reviewed, and strengthened where necessary, such that there is assurance with regard to institution and maintenance of high levels of basic infection prevention and control standards including in relation to promotion and facilitation of hand and respiratory hygiene, ventilation, and protection of employees and patrons.
- the NPHET gave specific consideration to the use of the COVID-19 pass. The NPHET noted the results of the recent SAM study from the ESRI which suggests that, notwithstanding the efforts of many businesses to adhere to sectoral guidelines, the COVID-19 pass has not been appropriately implemented across the hospitality sector in its entirety. Given the current trajectory of the disease, the NPHET strongly recommends that:
o compliance with this measure be reviewed and strengthened, along with the other protective measures currently recommended for the hospitality sector.
o In addition, the NPHET recommends that the COVID pass be implemented more widely and robustly than is currently the case, including in hospitality and for indoor events.
- homeworking has played a very important role in containing the spread of COVID-19 throughout the duration of the pandemic. With the easing of social and economic restrictions, a majority of employees have already or will need to return to the workplace on an at least partial basis over the coming months. This should continue to be phased and cautious and the NPHET continues to recommend that all who can work from home should continue to do so. All other protective measures currently in place, as set out in the Work Safely Protocol, should continue to be adhered to by workplaces, employers and employees. In particular, there is a need for an ongoing partnership approach between employers and employees to ensure that the importance of self-isolating when symptomatic is understood, communicated and facilitated, such that employees are not disincentivised to identify themselves as symptomatic and stay at home where appropriate.
The NPHET cautions that the re-imposition of public health restrictive measures may be warranted should the application of the above measures not have sufficient effect on the profile of disease. In this regard, compliance with basic public health measures by the general public and across sectors will be critical.
subject to operational feasibility that the COVID pass be adopted as a requirement for visitation to healthcare settings with a provision for exemptions on compassionate
grounds.
the Rapid Testing Expert Advisory Group be requested to examine the potential role and feasibility of rapid testing as a component of the COVID pass for those for whom,
on medical grounds, it is not been possible to get fully vaccinated.
As noted in its letter of 16th September 2021, in the context of the highly transmissible Delta variant, it is unlikely that vaccination alone, even at the high levels of vaccine coverage that we have now
achieved, will bring the effective reproduction number below 1 such that we will achieve suppression of the disease. This means that through this coming autumn and winter, possibly in the face of high levels of infection, we will remain dependent upon public understanding and buy-in to the basic public health measures in order to minimise opportunities for this virus to transmit. In this context,
NPHET noted the results of the most recent SAM study in relation to mitigative behaviours like
mask wearing, hand hygiene and keeping physical distance; while most people still recognise that
risk of infection is linked with how many people they meet and which locations they go to, the data suggests that people are discounting the potential value of mitigative behaviours in reducing their risk,
than one-quarter of people reporting that they are not engaging in mitigative behaviours
most of the time when leaving home. The NPHET therefore recommends that continuing efforts are made across all sectors to ensure clear guidance and communication with the public on the need for
the
with more
their
a cultural shift towards embedding individual and collective strategies to mitigate against COVID-19
and other respiratory infections.
This should involve a strengthening of the ongoing co-ordinated
approach to communications across Government and relevant agencies, ensuring a consistent and coherent message across Government, Department of Health, the NPHET, the HSE, and relevant agencies and sectors. As part of this, it is essential that workplaces, the retail sector, public transport operators, sporting and cultural organisations, and other public facing sectors review and, where
necessary, refresh their messaging, signage, and their provision of hand sanitiser.
The NPHET has previously outlined that planning for a transition from mass scale SARS-CoV-2 testing would be predicated on achievement of the criteria as set out above. Given that these criteria have not been met, the NPHET recommends that the current approach to the public health management of contacts and cases be maintained. In addition, given the high and increasing incidence of disease in the community, the NPHET has further recommended that, subject to operational feasibility, the HSE
should implement a programme of
COVID-19 antigen testing (with PCR confirmation of positive cases)
for people who are identified as fully vaccinated close contacts of a confirmed case and who do not
have any symptoms.
The NPHET recognised that, based on the above recommendations, all sectors of society will now be open and, as such, some individuals will engage in activities and behaviours which are higher risk. In
this context, the NPHET
recommended that the Rapid Testing Expert Advisory Group be requested to
provide a view as to the potential utility of voluntary self-testing by asymptomatic individuals who
plan to engage in such high-risk behaviours and activities.
The NPHET, of course, remains available to provide any further advice and recommendations that may be of assistance to you and Government in relation to ongoing decision-making processes in respect of the COVID-19 pandemic. As always, I would be happy to discuss further, should you wish.
Yours sincerely,
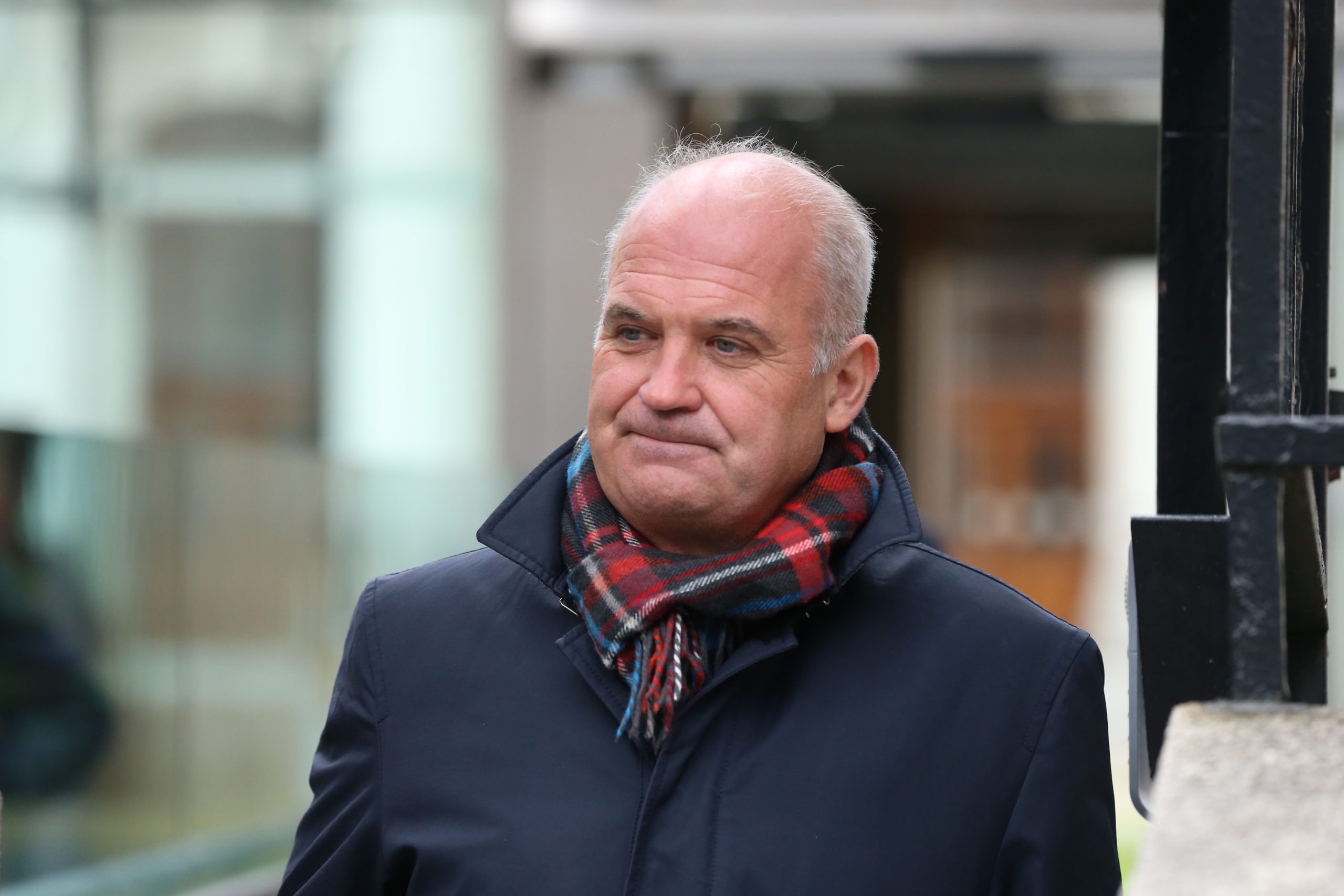
__________________________ Dr Tony Holohan
Chief Medical Officer
Chair of the COVID-19 National Public Health Emergency Team
cc. Ms Elizabeth Canavan, Department of the Taoiseach and Chair of the Senior Officials Group for COVID-19
8
Appendix 1: Supplementary Modelling Information
IEMAG has implemented an age-cohorted model, where the population is divided into six age groups (aged 0-12, 13-19, 20-24, 25-44, 54-64 and 65 and older) and contact within and between groups calibrated on the basis of international data on patterns of social contact. The spread of infection within the population is limited by this age structure, and as such this model tends to generate lower estimates of infection than the homogeneous model. At this point in the pandemic we have reason to believe that the estimates from the age-cohorted model are more accurate. The age-cohorted model also specifically allows us to model the opening of schools, as the contact patterns for children of school-going age can be switched between those expected during school term and those expected out-of-term.
Given that over 90% of adults are fully vaccinated, a key determinant of the spread of infection is the extent to which unvaccinated children transmit the virus. The models examine two fundamental scenarios, one where it is assumed that children and adults are equally likely to become infected and to transmit the virus, and one where it is assumed that children under 12 years of age are 50% as likely to transmit the virus as adults (low child transmission).
Within these scenarios, the models looked at a progressive increase in effective social contact in September and October 2021:
- a conservative scenario, where effective social contact at the end of October 2021 is similar to that seen in December 2020, but with the population maintaining basic non-pharmaceutical measures (such as self-isolating when symptomatic, good respiratory and hand hygiene, and masks in crowded settings) sufficient to interrupt about 30% of potential transmissions; and,
- a pessimistic scenario where effective social contact at the end of October 2021 reverts to pre-pandemic levels with few or no effective mitigation measures.
It should be noted that ‘effective social contact’ in these models is an estimate not only of the level of close social contact, but also the risk of transmission associated with those contacts, including the effectiveness of non-pharmaceutical interventions, and the changing risk of social contact in the winter compared to the summer.
Effective social contact increases in steps starting on 30/8/21 where schoolchildren switch to in-school contact patterns, increasing again on 20/9/21 to coincide with the return of higher education, a further step on 4/10/21, and the final step on 25/10/21.
The delta variant is assumed to have a transmission advantage of 1.97 over ancestral (wild-type) SARS- CoV-2, that is, delta is almost twice as transmissible. Vaccines are assumed to be 80-90% effective in preventing symptomatic infection, and 95% effective in preventing severe disease.
It is informative, rather than recalibrating and re-running these models, to see how they have performed since they were originally calibrated and run in August 2021.
The model scenarios are compared to actual case counts (black points) in Figure 1. The actual case counts have, since the end of August 2021, followed relatively closely the ‘low child transmission’ scenario, which accords with the international evidence that, at a population level, children transmit SARS-CoV-2 less effectively than adults. However, since early October 2020, case counts are following the more pessimistic scenario in terms of effective social contact, albeit about a week later than in the models. This indicates that the level of social contact is high, and that mitigation measures to reduce transmission are not sufficiently effective to suppress transmission, despite the very high levels of
9
vaccination. There are a number of possible reasons why we have deviated from the more conservative scenario towards the pessimistic: we know from the ESRI Social Activity Measure and mobility data that mobility and social contact are increasing, and adherence to infection prevention measures is decreasing. A shift in social mixing from outdoors to indoors may be playing a role.
The impact of these scenarios on the burden of severe disease and the demand for healthcare are shown in Figure 2 and Figure 3. The number of people in hospital is also now tracking the ‘pessimistic – low child transmission’ scenario, though again about one week later than in the model. Given that the delay between increasing cases and increased numbers of people in critical care is longer than for hospitalisation, we are now at the point where numbers in critical care might be expected to increase further. If we do continue to follow the ‘pessimistic – low child transmission’ scenario we could have 800-1000 people in hospital at a peak in mid-November, 150-200 requiring critical care and 700-800 requiring general hospital care. Under this scenario we could expect approximately 2,000 new admissions to hospital and over 300 admissions to ICU between now and the end of the year.
Figure 1: Age-cohorted SEIR model scenario estimates of new cases per day, run on 25 August 2021. Confidence intervals generated by stochastic variation in contact rates. The solid line is the ensemble average of all runs, dark ribbon the interquartile range, and the light ribbon the 2.5 and 97.5 percentiles. Grey points are actual case counts to calibration date, black points are case counts since the model was run. The effect of vaccination included according to latest vaccination data. Delta variant replaces alpha in July 2021, accounting for 70% of transmissions by 18 July 2021. Delta transmission advantage 1.97 over ancestral. School-children switch between out-of-school and in-school contact patterns based on the standard school year. Effective social contact increases in steps on 30/8/21 where school-children switch to in-school contact patterns, 20/9/21 , 4/10/21 and 25/10/21. The level of effective social contact at this point, in the conservative scenario is equivalent to that seen in December 2020, with basic non-pharmaceutical measures interrupting about 30% of transmissions; in the pessimistic scenario it is equivalent to a freely mixing society with no mitigation measures. Low child transmission scenarios assume children under 12 years of age to be 50% as likely to transmit the infection as adults.
Help support Cork Safety Alerts by becoming a member – Click Here